The inconvenient truth about Republican Medicaid fraud claims
Trump’s first 100 days have shown an administration committed to using fraud and waste as a false pretext for large spending cuts.

Few lines are more central to the congressional Republican leadership’s elevator pitch than the idea that we will get major savings by cutting Medicaid fraud, not Medicaid benefits.
This sales pitch is no small deal to this White House. A president seeking to pass his tax bill with slim congressional majorities could be tanked by a handful of Republicans afraid they’ll lose seats. Those seats could be at risk if Republicans are seen as paying for tax cuts to the most well-off by cutting Medicaid benefits for hard-pressed workers, children, seniors or families of children with disabilities.
No wonder the White House and Republican leadership are desperate to claim that there is a large pile of fraudulent and wasteful Medicaid spending that could be eliminated without forcing states to cut benefits or hurt rural hospitals.
Facts, however, are not kind to this claim. Independent oversight analysis shows a relatively small and declining amount of improper Medicaid payments, meaning that cutting hundreds of billions of dollars in Medicaid spending promised to states would inevitably lead to dramatic coverage loss and benefit cuts.
One particularly inconvenient truth is that estimates of “improper payments” — a category that includes not only fraud and mistaken payments but insufficient documentation — undermine Republican claims that Medicaid cuts will not lead to benefit cuts.
Both the independent inspector general’s office and the Governmental Accountability Office have found that the vast majority of Medicaid improper payments, around 80 percent in recent years, resulted not from fraud or waste, but from states having insufficient documentation to meet their paperwork requirements.
Another issue with the Republicans' argument is that, following the pandemic, when states had more flexibility in terms of paperwork requirements, the improper payment rate was cut by two-thirds to only 5.1 percent from 2022 to 2024 as states improved compliance efforts.
This is significant. Improper payment rates of 5 percent are comparable to the private sector, where estimates of fraud (not just a broad definition of improper payments) are around 3-5 percent.
Conservative advocates straining to call these smaller numbers into question are making an odd argument. They are essentially calling for more onerous paperwork and red tape while suggesting that every governor who reported low improper payments over the last several years — including leading Republican governors from Texas, Florida, Georgia and Indiana — used more flexible pandemic requirements to dramatically underreport improper payments.
Indeed, Trump’s first 100 days have shown an administration committed to using fraud and waste as a false pretext for large spending cuts, while taking actions that undermined anything that could be seen as a serious strategy to take on actual Medicaid fraud.
First, the White House and Republican leadership have focused on fraud by Medicaid beneficiaries, when Americans who receive Medicaid make up only 2 percent of Medicaid fraud convictions. The evidence shows that provider schemes by medical device companies, home health agencies, pharmacies and others constitute the overwhelming majority of Medicaid fraud.
Second, the White House and the Department of Government Efficiency have attacked the oversight community. These officials are critical to providing leads to federal prosecutors, fulfilling the Government Accountability Office’s “Medicaid Program Integrity” recommendations and strengthening Medicaid Fraud Control Units that investigate and prosecute providers in every state.
Instead of embracing oversight, Republicans belittled oversight officials while summarily firing the highly respected inspector general at the Department of Health and Human Services.
Third, rather than investing in cutting-edge technology and data-matching tools to detect and prevent the type of fraud that cost taxpayers billions in the first months of the pandemic, the White House chose sledgehammer cuts to Health and Human Services expertise while proposing no additional technological investments at the federal or state level.
Serious steps to take on Medicaid fraud are being ignored because they don’t further the White House strategy of denying states hundreds of billions of Medicaid funding and then shifting the blame to states when they are forced to cut benefits.
In addition to floating Medicaid cost caps and denying provider taxes that nearly all states legally use, Republican leaders seem intent on reducing Medicaid funding for the 20 million Americans with expanded coverage under the Affordable Care Act.
The Urban Institute estimates that pulling back this funding could reduce health coverage for up to 10 million working Americans, including 55 to 64-year-olds who fell into the trap of not being low-income enough for federal help or well-off enough to afford private insurance. Alternatively, the cuts can lead states to make up the costs by cutting “optional” Medicaid programs that provide prescriptions for children with autism and Down Syndrome and home care help for seniors.
With Medicaid’s improper payments down significantly and costs growing more slowly than the private sector, low reimbursement rates are already threatening the viability of rural hospitals. Even with current funding, there are painfully long wait lists for long-term care services for older Americans or children with disabilities.
There is no hiding the following inconvenient truth: Slashing Medicaid to offset tax cuts for well-off Americans will inevitably lead to deep cuts to Medicaid benefits, increase uncompensated visits to hospitals and physicians and swell the number of uninsured Americans by millions.
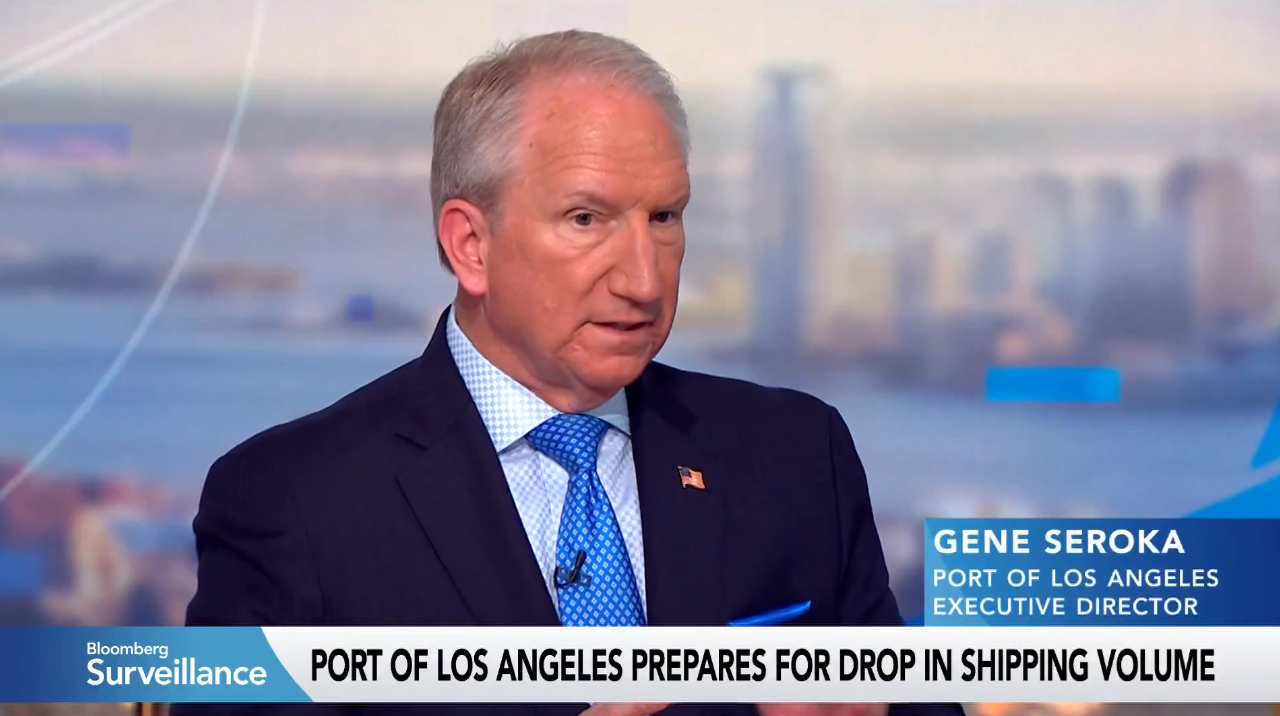
Gene Sperling is a former senior advisor to President Joe Biden and National Economic Council director to Presidents Barack Obama and Bill Clinton. Joshua Waldman is a former White House economic advisor to the American Rescue Plan.