How Legacy Systems Stifle Innovation in Healthcare
Legacy systems in healthcare, particularly outdated Electronic Health Record (EHR) systems, pose significant challenges to innovation, patient care, and the adoption of new technologies like Artificial Intelligence (AI). These old systems, which are no longer updated or supported, can hinder the integration of new tools and methods, ultimately affecting the quality of care provided to patients. What are Legacy EHR Systems? Legacy EHR systems are outdated software or technologies that are still in use but are not updated. They were designed to manage patient data, but their inability to integrate with new technologies and systems creates barriers to innovation and advancements in patient care. Barriers to Innovation Caused by Legacy EHR Systems Legacy EHR systems pose several barriers to innovation in healthcare, including: Data Format Issues: Legacy EHR systems may store data in formats that are not compatible with new technologies, such as AI and machine learning. Lack of APIs: Outdated EHR systems may not have Application Programming Interfaces (APIs) that allow new software to connect and retrieve data. Security Concerns: Legacy EHR systems may not have the necessary security measures to protect sensitive patient data, making it difficult to integrate new technologies. Inability to Support Real-Time Data Access: Legacy EHR systems may not be able to support real-time data access, making it difficult to implement AI-driven predictive analytics. Manual Data Entry: Legacy EHR systems may require manual data entry, which can be time-consuming and take away from healthcare providers' ability to focus on patient care. Incompatibility with New Technologies: Legacy EHR systems may not be compatible with new technologies, such as wearable devices and mobile health applications. Limited Scalability: Legacy EHR systems may not be able to scale to meet the growing needs of healthcare organizations, making it difficult to implement new technologies. Problems Caused by Legacy EHR Systems Some of the key problems caused by legacy EHR systems include: Delayed AI adoption: Legacy EHR systems may not be compatible with AI tools, slowing down the adoption of AI in healthcare. Interoperability issues: Outdated EHR systems may not be able to communicate with other systems, leading to fragmented care and errors. Hindered patient care advancements: Legacy EHR systems may not support new treatment methods or data analysis techniques, delaying patient care advancements. Case Studies: The Impact of Legacy EHR Systems Several case studies illustrate the impact of legacy EHR systems on innovation, AI adoption, and patient care. For example: The Veterans Health Administration's transition from their legacy VistA system to a modern Cerner EHR faced challenges with interoperability and data migration, affecting their ability to integrate new technologies. A hospital that couldn't participate in a regional health information exchange due to their EHR's inability to communicate with other systems, leading to delays in patient care. The UK's NHS struggles with legacy IT systems, which hindered their ability to track COVID-19 cases and distribute vaccines effectively. Statistics and Quotes Statistics show that a significant percentage of hospitals still use legacy systems, leading to increased costs due to inefficiencies. Healthcare professionals often express frustration with these systems, citing their inability to support new technologies and methods. Solutions to the Problem Possible solutions to the problem of legacy EHR systems include: Upgrading EHR systems to modern, cloud-based solutions that offer better integration and support for new technologies. Using middleware to bridge old and new technologies, enabling the integration of AI tools and other new systems. Adopting cloud-based solutions that offer better integration and support for new technologies. The Importance of Modernization Modernizing EHR systems is critical to enabling innovation in healthcare, improving patient outcomes, and ensuring seamless interoperability between different healthcare providers. A legacy software modernization company can help healthcare organizations upgrade their EHR systems, ensuring they are compatible with new technologies and can support advancements in patient care. Conclusion EHR systems pose significant challenges to innovation, patient care, and the adoption of new technologies in healthcare. Case studies illustrate the impact of these systems on AI adoption, interoperability, and patient care advancements. Modernizing EHR systems is critical to enabling innovation, improving patient outcomes, and ensuring seamless interoperability between different healthcare providers.
Legacy systems in healthcare, particularly outdated Electronic Health Record (EHR) systems, pose significant challenges to innovation, patient care, and the adoption of new technologies like Artificial Intelligence (AI). These old systems, which are no longer updated or supported, can hinder the integration of new tools and methods, ultimately affecting the quality of care provided to patients.
What are Legacy EHR Systems?
Legacy EHR systems are outdated software or technologies that are still in use but are not updated. They were designed to manage patient data, but their inability to integrate with new technologies and systems creates barriers to innovation and advancements in patient care.
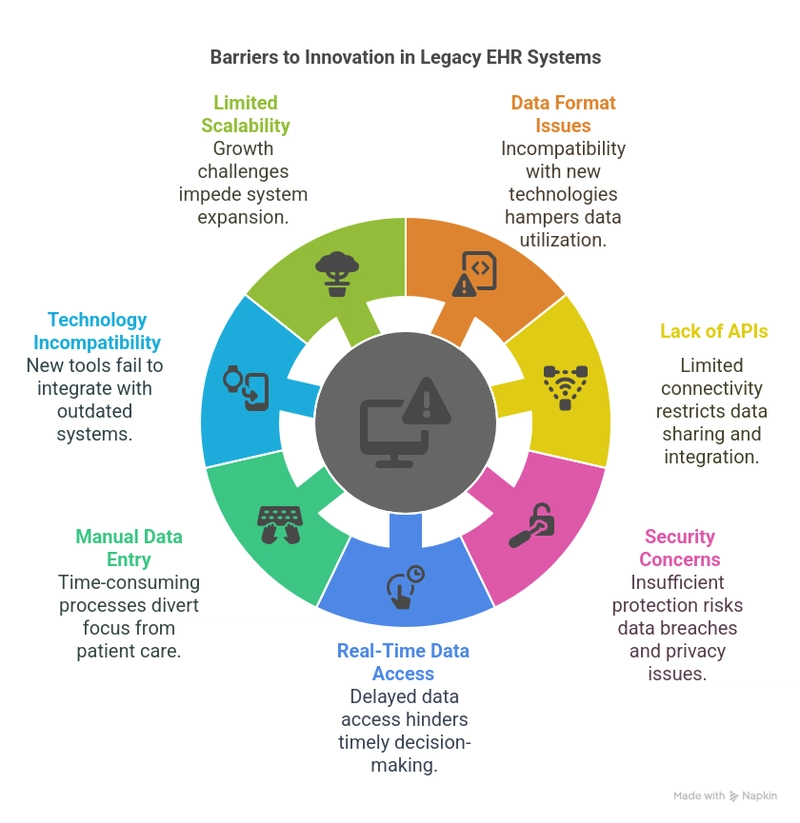
Barriers to Innovation Caused by Legacy EHR Systems
Legacy EHR systems pose several barriers to innovation in healthcare, including:
- Data Format Issues: Legacy EHR systems may store data in formats that are not compatible with new technologies, such as AI and machine learning.
- Lack of APIs: Outdated EHR systems may not have Application Programming Interfaces (APIs) that allow new software to connect and retrieve data.
- Security Concerns: Legacy EHR systems may not have the necessary security measures to protect sensitive patient data, making it difficult to integrate new technologies.
- Inability to Support Real-Time Data Access: Legacy EHR systems may not be able to support real-time data access, making it difficult to implement AI-driven predictive analytics.
- Manual Data Entry: Legacy EHR systems may require manual data entry, which can be time-consuming and take away from healthcare providers' ability to focus on patient care.
- Incompatibility with New Technologies: Legacy EHR systems may not be compatible with new technologies, such as wearable devices and mobile health applications.
- Limited Scalability: Legacy EHR systems may not be able to scale to meet the growing needs of healthcare organizations, making it difficult to implement new technologies.
Problems Caused by Legacy EHR Systems
Some of the key problems caused by legacy EHR systems include:
- Delayed AI adoption: Legacy EHR systems may not be compatible with AI tools, slowing down the adoption of AI in healthcare.
- Interoperability issues: Outdated EHR systems may not be able to communicate with other systems, leading to fragmented care and errors.
- Hindered patient care advancements: Legacy EHR systems may not support new treatment methods or data analysis techniques, delaying patient care advancements.
Case Studies: The Impact of Legacy EHR Systems
Several case studies illustrate the impact of legacy EHR systems on innovation, AI adoption, and patient care. For example:
- The Veterans Health Administration's transition from their legacy VistA system to a modern Cerner EHR faced challenges with interoperability and data migration, affecting their ability to integrate new technologies.
- A hospital that couldn't participate in a regional health information exchange due to their EHR's inability to communicate with other systems, leading to delays in patient care.
- The UK's NHS struggles with legacy IT systems, which hindered their ability to track COVID-19 cases and distribute vaccines effectively.
Statistics and Quotes
Statistics show that a significant percentage of hospitals still use legacy systems, leading to increased costs due to inefficiencies. Healthcare professionals often express frustration with these systems, citing their inability to support new technologies and methods.
Solutions to the Problem
Possible solutions to the problem of legacy EHR systems include:
- Upgrading EHR systems to modern, cloud-based solutions that offer better integration and support for new technologies.
- Using middleware to bridge old and new technologies, enabling the integration of AI tools and other new systems.
- Adopting cloud-based solutions that offer better integration and support for new technologies.
The Importance of Modernization
Modernizing EHR systems is critical to enabling innovation in healthcare, improving patient outcomes, and ensuring seamless interoperability between different healthcare providers. A legacy software modernization company can help healthcare organizations upgrade their EHR systems, ensuring they are compatible with new technologies and can support advancements in patient care.
Conclusion
EHR systems pose significant challenges to innovation, patient care, and the adoption of new technologies in healthcare. Case studies illustrate the impact of these systems on AI adoption, interoperability, and patient care advancements. Modernizing EHR systems is critical to enabling innovation, improving patient outcomes, and ensuring seamless interoperability between different healthcare providers.