Congress can improve postpartum care
Pelvic floor physical therapy can be effective in treating postpartum disorders such as urinary and fecal incontinence, pelvic organ prolapse, pelvic pain and sexual dysfunction, and should be covered by Medicaid for 12 months to ensure new mothers receive the appropriate care.

A study surveying mothers nine to 12 months postpartum found that more than two-thirds of women reported at least one physical health problem since childbirth. This can include backaches, incontinence, fatigue, abdominal pain and painful intercourse. These problems are highly correlated to functional limitations such as childcare, work and daily activities. Despite this, many women struggle to get appropriate health care.
Typically, in the U.S., after a woman gives birth, the next follow up will be in six weeks. But for many women, physical symptoms from birth will persist beyond this period. During pregnancy, the pelvic floor and abdominal muscles are stretched and weakened. These changes can cause multiple musculoskeletal disorders that go untreated.
While many people know physical therapists can treat low back pain and fatigue, they may be unaware that physical therapists can also treat other conditions, such as urinary and fecal incontinence, pelvic organ prolapse, pelvic pain and sexual dysfunction. Pelvic floor physical therapy is not just performing kegels; physical therapists can work with patients to strengthen, relax or activate pelvic floor muscles to return to their previous function.
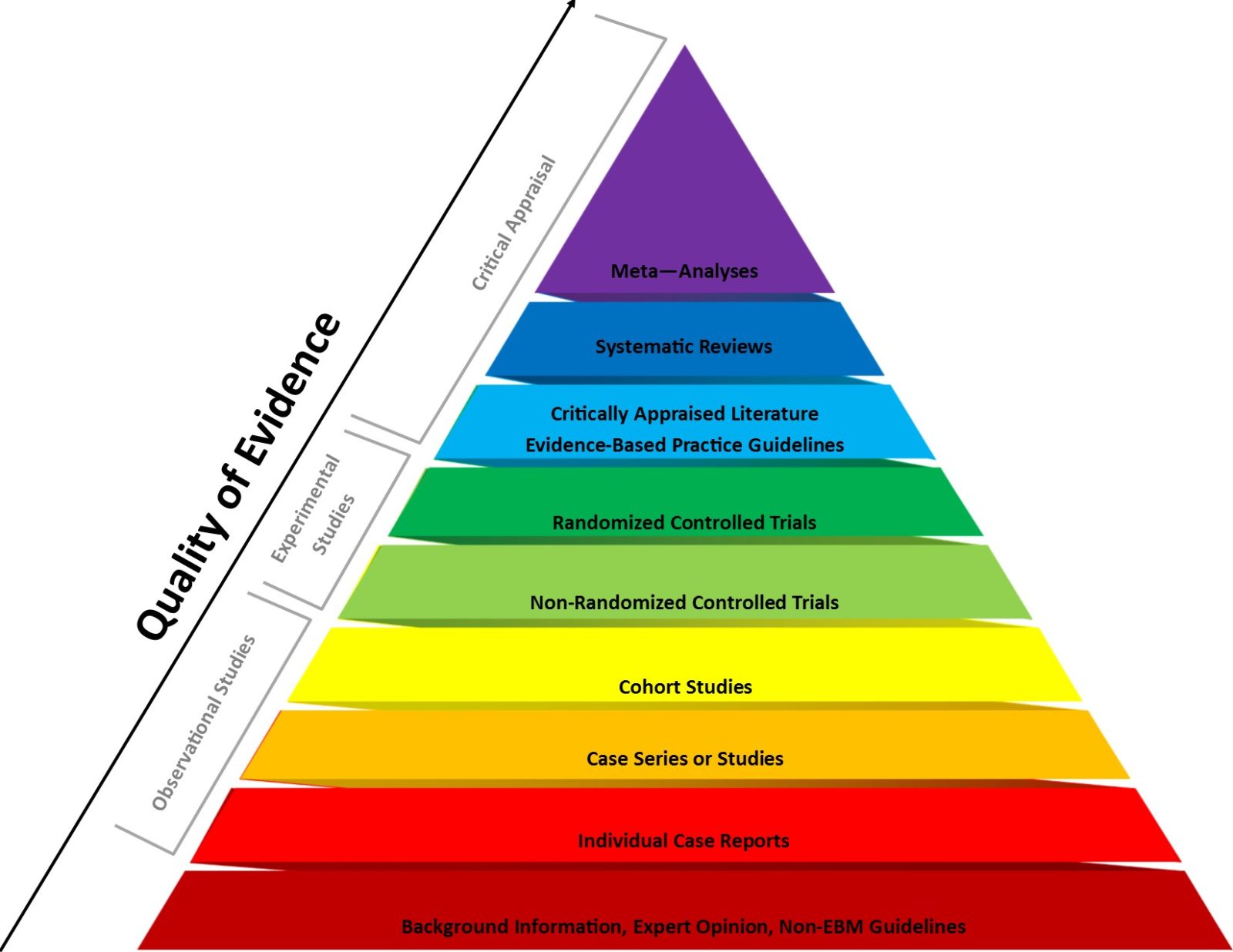
Several studies show physical therapy is, “effective in increasing pelvic floor muscle strength and endurance, reducing incontinence symptoms, pelvic organ prolapse, and sexual dysfunction.” A systematic review found that women who received pelvic floor physical therapy were five to eight times more likely to recover from urinary incontinence than women that did not. Physical therapy is shown to be effective for conservative management postpartum disorders.
Though there are many benefits that physical therapy has to offer postpartum women, there are several barriers to access. There is a social stigma related to discussing issues about our pelvic floors. Women may not be comfortable discussing urinary or fecal incontinence, sexual dysfunction or pelvic pain.
Because of this, new parents may not even know that the dysfunctions they are experiencing are not normal. As a current physical therapy student, I have seen the power of patient education and listening. Making sure the patient is heard can make all the difference for someone who is experiencing pain.
Even if women do know about physical therapy, it can be expensive and their insurance may not cover enough visits. Currently, women lose their Medicaid benefits after 60 days. To address these problems, Medicaid should expand their coverage of postpartum care. The Optimizing Postpartum Outcomes Act addresses Medicare and Medicaid services for prenatal and postpartum pelvic health services. It would expand Medicaid coverage to 12 months and provide coverage for rehabilitation and mental heath services. Expanding coverage and care can help new mothers gain access to better care.
Though it may seem like another major health care cost to the U.S., this act may actually save money for the health care industry in the long run. There is a shortage of obstetric care in the U.S. Physical therapists can help alleviate the load for obstetricians by addressing musculoskeletal issues postpartum. Not only for physical health concerns but mental health issues that may arise.
As a student, I am trained to look for not only red flags but also mental health concerns to be able to provide appropriate referrals if needed. A new generation of physical therapists and obstetricians can work together to provide care from new mothers.
Catching these issues early on can save a considerable amount of money down the line when it comes to dealing with chronic health concerns like chronic low back pain and chronic pelvic pain which cost the U.S. billions of dollars a year.
I urge leaders in Congress to take the steps to ensuring that women's postpartum care is expanded and appropriate care is taken to decrease the economic burden of chronic disease.
Christine Nguyen is a Doctor of Physical Therapy student from Texas Woman's University.